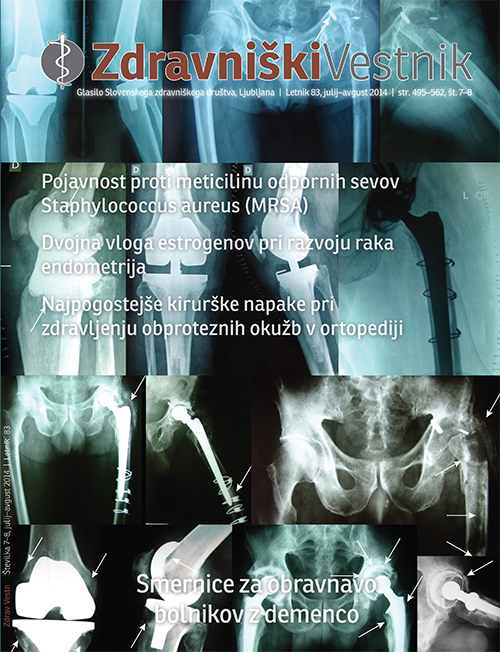
Most common surgical mistakes with treatment of prosthetic joint infections
Abstract
The treatment of infections of orthopedic implants is often difficult and complex, although the chances of successful treatment with properly selected diagnostics, surgical and antibiotic treatment protocol have recently increased significantly. Surgical treatment is a key stone factor in the treatment of infections of orthopedic implants and any errors in it often lead to worse clinical outcomes. The most important and frequent surgical errors include: conservative treatment of periprothetic infections with antibiotics only, to-late surgical revision, insufficient debridement during surgical revision, inadequate intraoperative samples for bacteriological and histological analysis. It is important to have and to follow proper treatment algorithm for periprosthetic joint infection. In this work we present the listed surgical and most illustrative key errors.
Downloads
References
Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 2010; 468: 45-51.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic joint infections. N Eng J Med 2004; 351: 1645-1654.
Moran E, Byren I, Atkins BL. The diagnosis and management of prosthetic joint infections. J Antimicrob Chemother 2010; 65 (suppl 3): iii45-iii54.
Darouiche R. Treatment of infections associated with surgical implants. N Engl J Med 2004; 350: 1422-1429.
Kurtz SM, Lau E, Schmier J, et al. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008; 23: 984-91.
Klouche S, Sariali E, Mamoudy P. Total hip arthroplasty revision due to infection: a cost analysis approach. Orthop Traumatol Surg Res 2010 Apr; 96 (2): 124-132.
Berbari EF, Hanssen AD, Duffy MC, et al. Risk factors for prosthetic joint infection: case-control study. Clin Infect Dis 1998; 27: 1247–1254.
Marculescu CE, Berbari FE, Hanssen AD, Steckelberg JM, Harmsen SW, Mandrekar JN, et al. Outcome of Prosthetic Joint Infections Treated with Debridement and Retention of Components. Clin Infect Dis 2006; 42 (4): 471-478.
Wymenga AB, van Horn JR, Theeuwes A, Muytjens HL, Slooff TJ. Perioperative factors associated with septic arthritis after arthroplasty. Prospective multicenter study of 362 knee and 2651 hip operations. Acta Orthop Scand 1992; 63: 665–671.
Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science 1999; 284: 1318-1322.
Gristina A, Naylor P, Myrvik Q. Infections from biomaterials and implants: a race for the surface. Med Prog Technol 1988; 14: 205-224.
Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet 2001; 358: 135–138.
Costerton JW, Lewandowski Z, Caldwell DE, Korber DR, Lappin-Scott HM. Microbial biofilms. Annu Rev Microbiol 1995: 711–745.
Lentino JR. Prosthetic Joint Infections: Bane of Orthopedists, Challenge for Infectious Disease Specialists. Clin Infect Dis 2003; 36 (9): 1157-1161.
Maurer TB, Ochsner PE. Infekt nach Knietotalprothesenimplantation. Zweizeitiger Wechsel als Element des Liestaler Behandlungsalgorithmus. Orthopade 2006 Sep; 35 (9): 917-8, 920-8.
Steckelberg JM, Osmon DR. Prosthetic joint infection. In: Waldvogel FA, Bisno AL, eds. Infections associated with indwelling medical devices. Third ed. Washington DC: American Society for Microbiology; 2000: 173-209.
Trebše R, Pišot V, Trampuž A. Treatment of infected retained implants. JBJS 2005; 87-B: 249-256.
Berbari EF, Hanssen AD, Duffy MC, et al. Risk factors for prosthetic joint infection: case-control study. Clin Infect Dis 1998; 27: 1247–1254.
Schafroth M, Zimmerli W, Brunazzi M, Ochsner PE. Infections. In: Ochsner PE, ed. Total hip replacement. Implantation technique and local complications. Berlin: Springer-Verlag; 2003: 65-90.
Trampuž A, Piper KE, Jacobson MJ et al. Sonication of removed hip and knee prostheses for diagnosis of infection. N Eng J Med 2007; 357: 654-663.
Parvizi J GE, Menashe S, Barrack RL, Bauer TW. Periprosthetic infection: what are the diagnostic challenges? J Bone Joint Surg [Am] 2006; 88-A: 138-147.
Berbari E, Marculescu C, Sia I et al. Culture negative prosthetic joint infection. Clin Infect Dis 2007; 45: 1113-1119.
Dolinar D, Koritnik B, Meglič J, Lotrič S. Preprečevanje in principi zdravljenja proteznih okužb v ortopediji. ZdravVestn 2007; 76: 117-124.
Aggarwal VK, Higuera C, Deirmengian G, Parvizi J, Austin MS. Swab cultures are not as effective as tissue cultures for diagnosis of periprosthetic joint infection.Clin Orthop Relat Res. 2013 Oct; 471(10): 3196-3203.
Font-Vizcarra L, García S, Bori G, Martinez-Pastor JC, Zumbado A, Morata L, Mensa J, Soriano A. Long-term results of acute prosthetic joint infection treated with debridement and prosthesis retention: a case-control study. Int J Artif Organs. 2012 Oct; 35(10): 908-912.
Trisha N. Peel, Kirsty L. Buising, Peter F.M. Choong. Diagnosis and Management of Prosthetic Joint Infection. Curr Opin Infect Dis. 2012; 25(6): 670-676.
McDonald D, Fitzgerald RJ, Ilstrup D. Two-stage reconstruction of a total hip arthroplasty because of infection. J Bone Joint Surg Am 1989; 71: 828-834.
Byren I, Bejon P, Atkins B, Angus B, Masters S, McLardy-Smith P, et al. One hundred and twelve infected arthroplasties treated with ‘DAIR’ (debridement, antibiotics and implant retention): antibiotic duration and outcome. J Antimicrob Chemother 2009; 63: 1264-1271.
Trampuž A, Zimmerli W. Prosthetic joint infections: update in diagnosis and treatment. Swiss Med Wkly 2005; 135: 243-251.
Wongworawat MD. Clinical faceoff: One- versus two-stage exchange arthroplasty for prosthetic joint infections. Clin Orthop Relat Res. 2013 Jun; 471(6): 1750-1753.
Schmitz HC, Schwantes B, Kendoff D. One-stage revision of knee endoprosthesis due to periprosthetic infection and Klippel-Trenaunay syndrome. Orthopade 2011; 40: 624-629.
Fleischmann W, Strecker W, Bombelli M, Kinzl L. Vacuum sealing as treatment of soft tissue damage in open fractures. Unfallchirurg 1993; 96(9): 488-492.
Kelm J, Schmitt E, Anagnostakos K. Vacuum-assisted closure in treatment of early hip joint infections. Int J Med Sci 2009; 6: 241-246.
EL Andaloussi S, Mäger I, Breakefield XO, Wood MJ. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov 2013; 12(5): 347-357.
Ogorevc E, Kralj-Iglič V, Veranič P. The role of extracellular vesicles in phenotypic cancer transformation. Radiol oncol 2013; 47 (3): 197-205.
Ogorevc E, Hudoklin S, Veranič P, Kralj-Iglič V. Extracellular vesicle-mediated transfer of membranous components from the highly malignant T24 urinary carcinoma cell line to the non-malignant RT4 urinary papilloma cell line. Protoplasma 2013; 10: 1-4.
Kralj-Iglič V. Stability of membranous nanostructures : a possible key mechanism in cancer progression. Int J Nanomedicine 2012; 7: 3579–3596.
Schara K, Janša V, Šuštar V, Dolinar D, Pavlič JI, Lokar M, et al. Mechanisms for the formation of membranous nanostructures in cell-to-cell communication. Cell Mol Biol 2009; 14 (4): 636-656.
Mrvar Brečko A, Šuštar V, Janša V, Štrukelj R, Janša R, Mujagić E, et al. Isolated microvesicles from peripheral blood and body fluids as observed by scanning electron microscope. Blood Cells Mol Dis 2010; 44(4): 307-312.
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, e tal. Executive summary: Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013 Jan; 56(1): 1-10.
Della Valle C, Parvizi J, Bauer TW, et al. Diagnosis of periprosthetic joint infections of the hip and knee. J Am Acad Orthop Surg 2010; 18: 760-770.
Haleem AA, Berry DJ, Hanssen AD. Mid-term to long-term followup of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res 2004; 428: 35-39.
Azzam K, McHale K, Austin M, Purtill JJ, Parvizi J. Outcome of a second two-stage reimplantation for periprosthetic knee infection. Clin Orthop Relat Res 2009; 467: 1706-1714.
Buechel FF, Femino FP, D’Alessio J. Primary exchange revision arthroplasty for infected total knee replacement: a long-term study. Am J Orthop (Belle Mead NJ) 2004; 33: 190-198.

The Author transfers to the Publisher (Zdravniški vestnik/Slovenian Medical Journal) all economic copyrights following form Article 22 of the Slovene Copyright and Related Rights Act (ZASP), including the right of reproduction, the right of distribution, the rental right, the right of public performance, the right of public transmission, the right of public communication by means of phonograms and videograms, the right of public presentation, the right of broadcasting, the right of rebroadcasting, the right of secondary broadcasting, the right of communication to the public, the right of transformation, the right of audiovisual adaptation and all other rights of the author according to ZASP.
The aforementioned rights are transferred non-exclusively, for an unlimited number of editions, for the term of the statutory
The Author can make use of his work himself or transfer subjective rights to others only after 3 months from date of first publishing in the journal Zdravniški vestnik/Slovenian Medical Journal.
The Publisher (Zdravniški vestnik/Slovenian Medical Journal) has the right to transfer the rights, acquired parties without explicit consent of the Author.
The Author consents that the Article be published under the Creative Commons BY-NC 4.0 (attribution-non-commercial) or comparable licence.